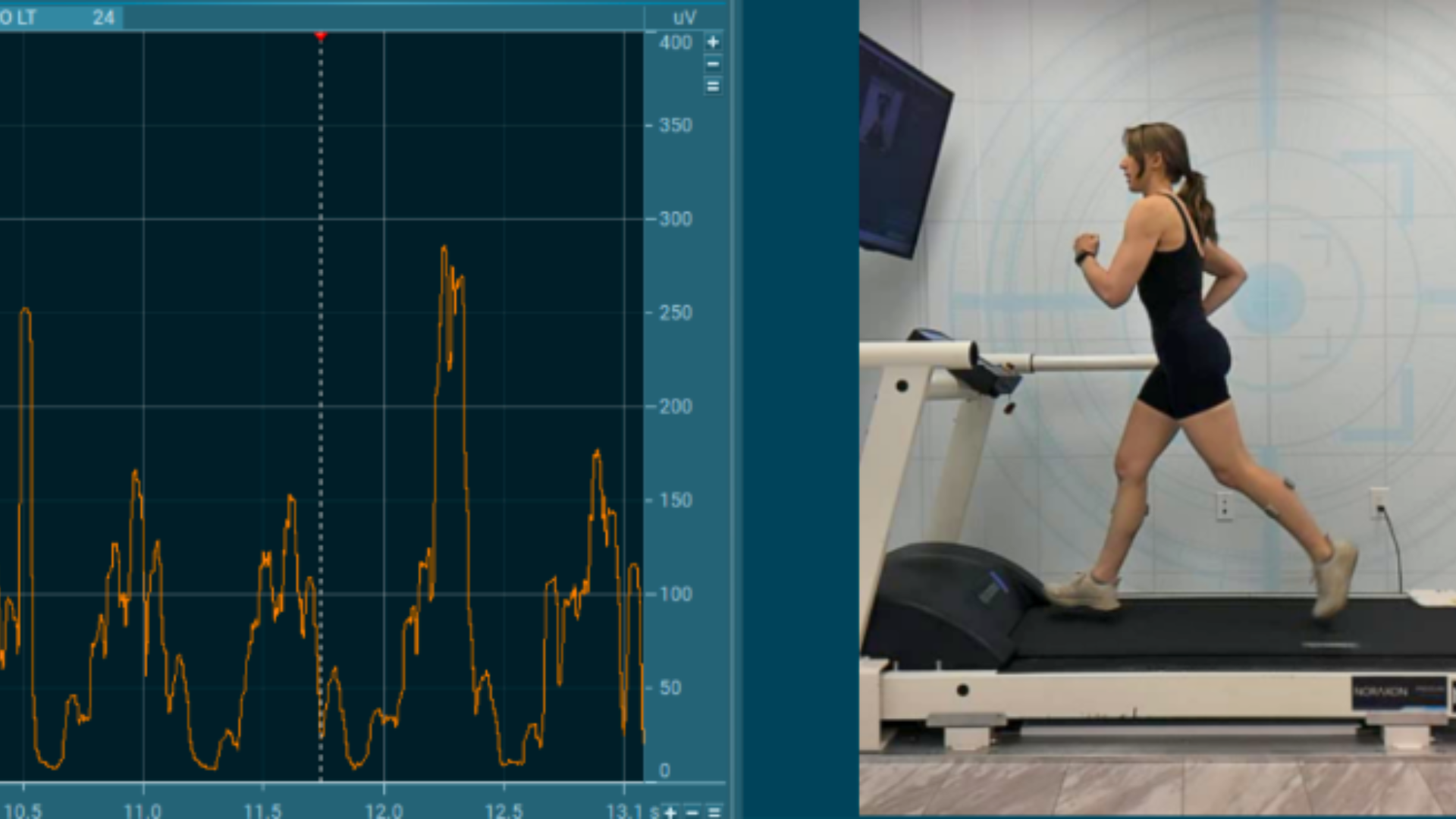
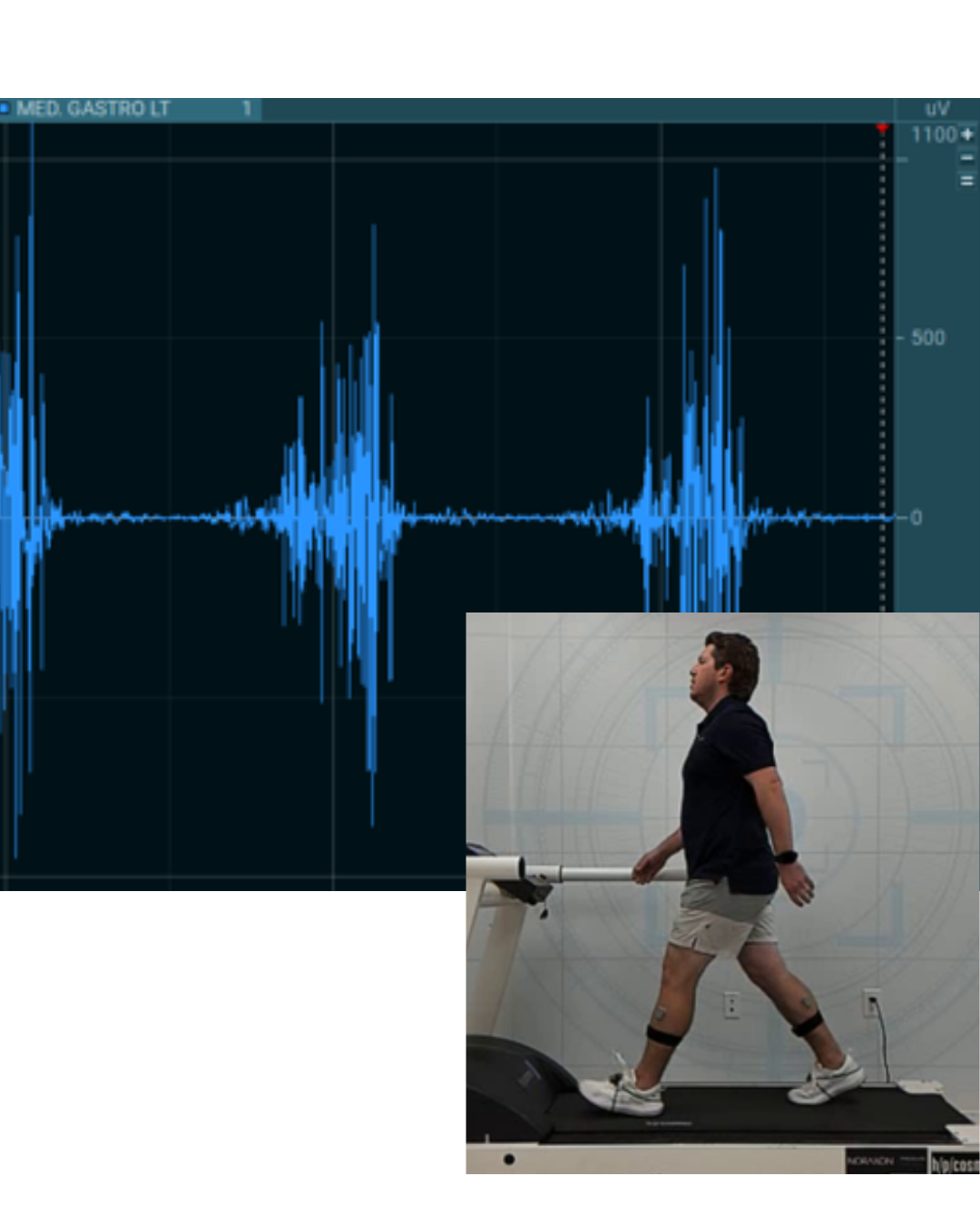
Electromyography (EMG) captures valuable data about muscle activity, but the raw signal is noisy, variable, and difficult to interpret without proper processing.
This article outlines the most common EMG processing techniques, explains when and why to apply them, and incorporates practical implementation details from Noraxon’s MR software platform
Filtering: The First Step
Why Filter?
Filtering is essential for cleaning up raw EMG signals by removing unwanted noise and signal artifacts. Surface EMG is susceptible to both:
- Low-frequency noise such as motion artifacts and DC offset
- High-frequency noise such as ambient electrical interference
So Why Does This Matter For EMG Analysis?
The answer is simple — motion artifact interferes with onset baseline evaluation and amplitude. Therefore, a high-pass filter may be needed any time motion artifact is noticed. This can be when:
- Recording high-movement activities (e.g. pitching, jumping).
- Using wireless EMG systems with cables or housing attached, as heavier objects attached to the electrode cause more motion artifact.
- Analyzing onset timing, where baseline stability matters.
Tradeoff: A higher cutoff may distort low-intensity muscle signals, so it’s a balance between noise reduction and preserving valid EMG content.
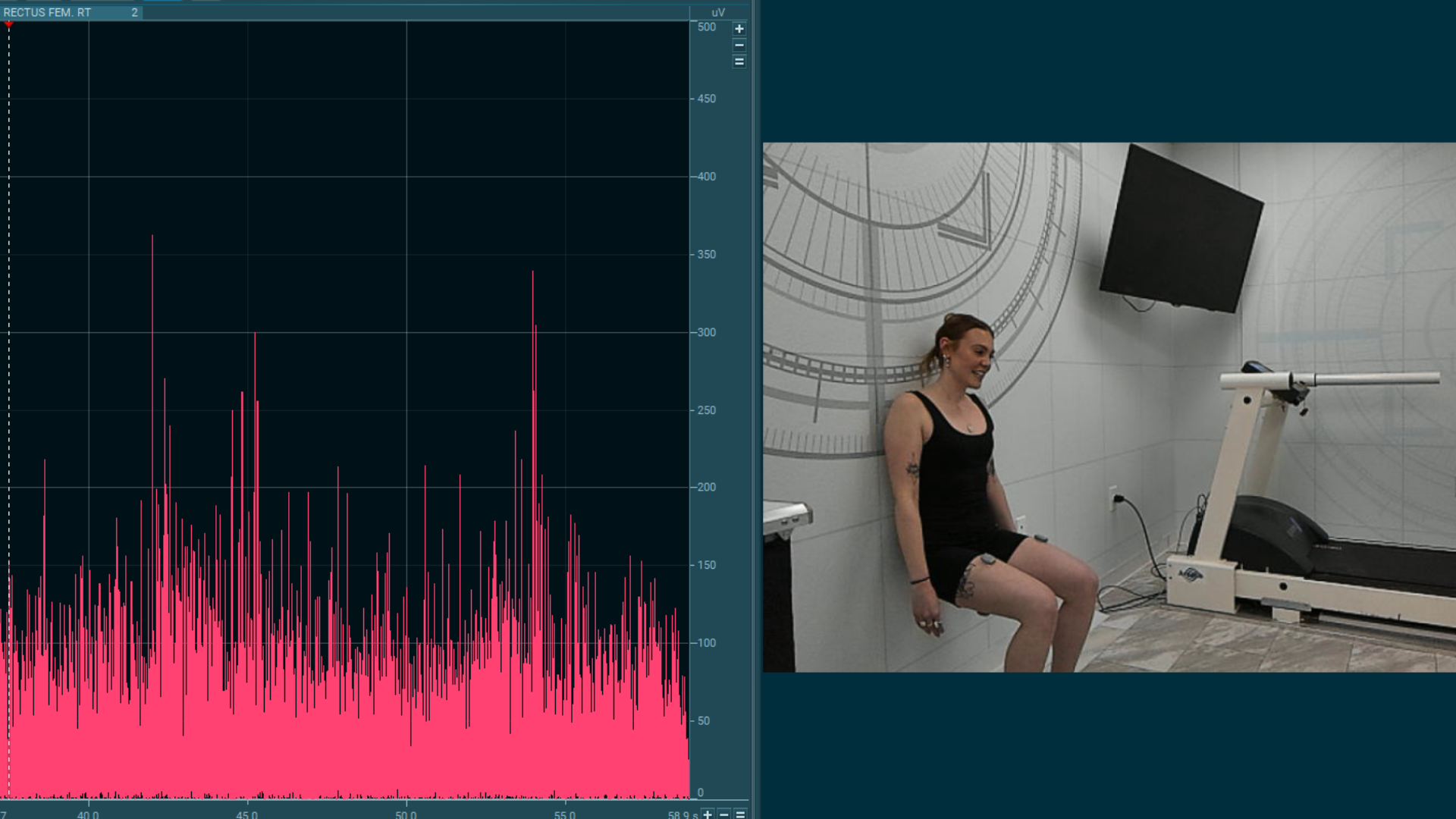
Rectification: Preparing the Signal for Amplitude Analysis
What is Rectification?
Rectification converts the EMG signal to absolute values, so all negative voltages become positive. This simplifies analysis and enables averaging.
- If a signal is not rectified before analyzing the amplitude, positive and negative values would otherwise cancel out.
- In MR, rectification is applied after filtering and before smoothing.
When Rectification Is Needed
Rectification is still required if you’re using:
- Moving average of mean absolute smoothing
- Calculating features like mean amplitude or area under the curve
Smoothing: Making Sense of EMG Amplitude
Why Apply Smoothing?
EMG signals are noisy by nature. Smoothing emphasizes the underlying envelope of activation and reduces point-to-point variability.
Common Algorithms
- RMS (Root Mean Square) – Reflects power of the signal over a window; most commonly used.
- Moving Average – Averages the rectified signal across a time window.
- Mean Absolute – Similar to moving average, but includes combined rectification.
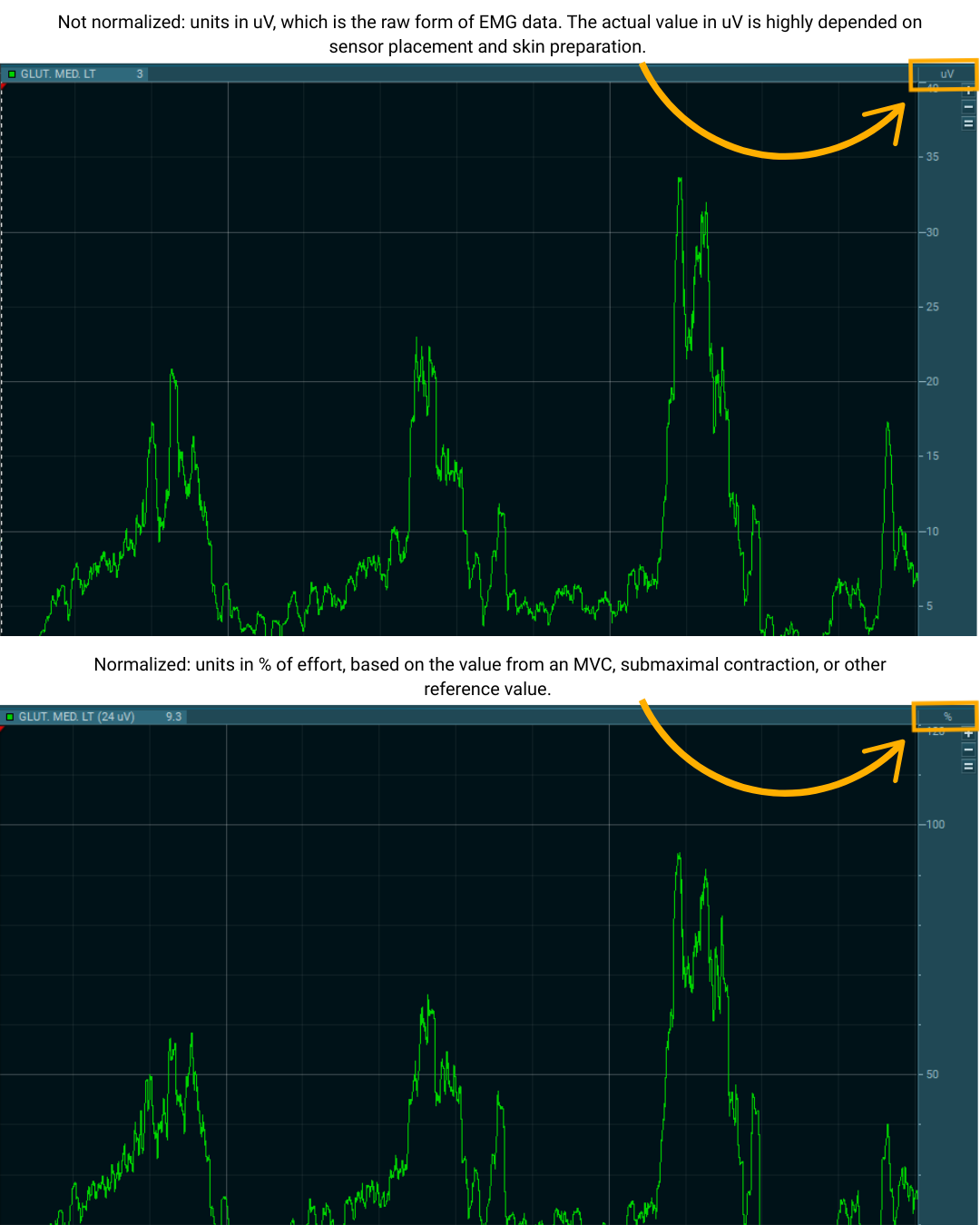
Amplitude Normalization — Making EMG Data Comparable
A major drawback of any EMG analysis is that the amplitude (microvolt scaled) data are strongly influenced by the given detection condition.
One solution to overcome this “uncertain” characteristic of micro-volt scaled parameters is the normalization to a reference value, e.g. the maximum voluntary contraction (MVC) value of a reference contraction. The basic idea is to “calibrate” the EMG signal in microvolts to a unique calibration unit with physiological relevance — the “percent of maximum innervation capacity” in that particular sense.
Other methods normalize to the internal mean value or a given trial or to the EMG level of a certain submaximal reference activity. The main effect of all normalization methods is that the influence of the given detection condition is eliminated and data are rescaled from microvolt to percent of selected reference value. It is important to understand that amplitude normalization does not change the shape of EMG curves, only their Y-axis scaling.
Summary: Best Practices for EMG Signal Processing
The techniques outlined in this article—filtering, rectification, smoothing, ECG reduction, and normalization—form the core of standard EMG signal processing. While these methods address the most common steps needed to prepare EMG data for analysis, this is not a comprehensive guide. For a deeper understanding of EMG theory, signal characteristics, and advanced analysis methods, users are encouraged to reference the ABC of EMG by Dr. Peter Konrad, and read the full article containing practical recommendations, linked below.

